5 Signs you should consult a podiatrist
Often, when we get a pain in our body, we may dismiss it, but you shouldn’t have to live with that crazy discomfort! Listen to your body and react when it pains you. If your feet, ankles or knees are aching, it may be a sign you need to consult a podiatrist. In the article below, we’ve included a few more signs to look out for too.
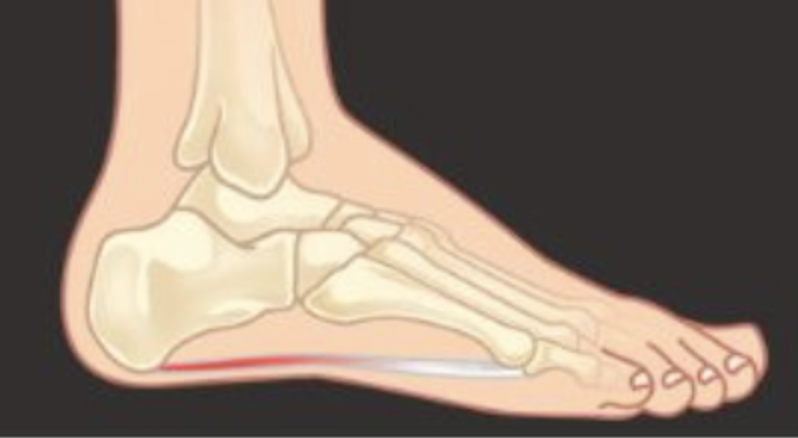
1. Heel Pain
It’s important to diagnose and resolve heel pain before it causes further complications – and considering that heel pain is often simply resolved, you should consult a podiatrist if you’re experiencing it.
Often factors like poor footwear, weight, biomechanics or particular walking and exercise styles contribute to heel pain, but thankfully, these can all be treated. Podiatrists help many with heel pain return to their usual, pain-free selves, whether they’re children or adults.
2. Sore, aching and tired feet
You shouldn’t have to live with a problem that can be easily solved, so if your feet are sore, aching or often tired, it’s time to consult a podiatrist. From advising you on which footwear is best for your situation to focusing on contributing factors, podiatrists are trained in resolving the aches and soreness that your feet may have.
3. Ingrown toenails
Ingrown toenails develop for many reasons: tight shoes, overly short nail trimming, and even trauma, such as hitting a toenail on something. Whatever the reason, ingrown toenails are sore, painful and thankfully, treatable.
If you currently have an ingrown toenail or tend to have them, a visit to the podiatrist is recommended. They can offer you conservative treatments, such as recommending specific shoes to wear, or surgical treatments, which will ease the pain by removing part of the nail.
4. Being a Diabetes patient
Foot health is commonly affected by diabetes, which is why you should include visits to a podiatrist as part of your management plan. They can conduct assessments testing the nerves and feet’s vascular supply. If there are any changes, they can be dealt with quickly, but these visits also act preventatively, as your podiatrist can guide you on how to avoid future complications.
This may range from recommended shoe styles to general foot and nail care techniques.
5. Bony deformities such as Bunions
If you have bunions and/or hammertoes, a podiatrist can take steps to decrease the amount of pain you experience. This is done by identifying the source of the pain and discussing treatment options. Although surgery is available, it may not always be necessary.
Contact us today
Whether you have ingrown toenails or bunions, you shouldn’t have to live with them untreated: a podiatrist can help you. Don’t wait until these matters get worse, contact us today and we will help you start your journey to better foot health.
We at the Foot Pod are passionate about good foot care and helping others achieve it. Whether you have a question about any of the above conditions or would like to book in for a regular check, we would be happy to assist. We are available online and by calling (08) 9246 7292.